Dermacuro Pain Blocker Vibration Neural Distraction Device
What is the Dermacuro Pain Blocker Vibration Neural Distraction Device?
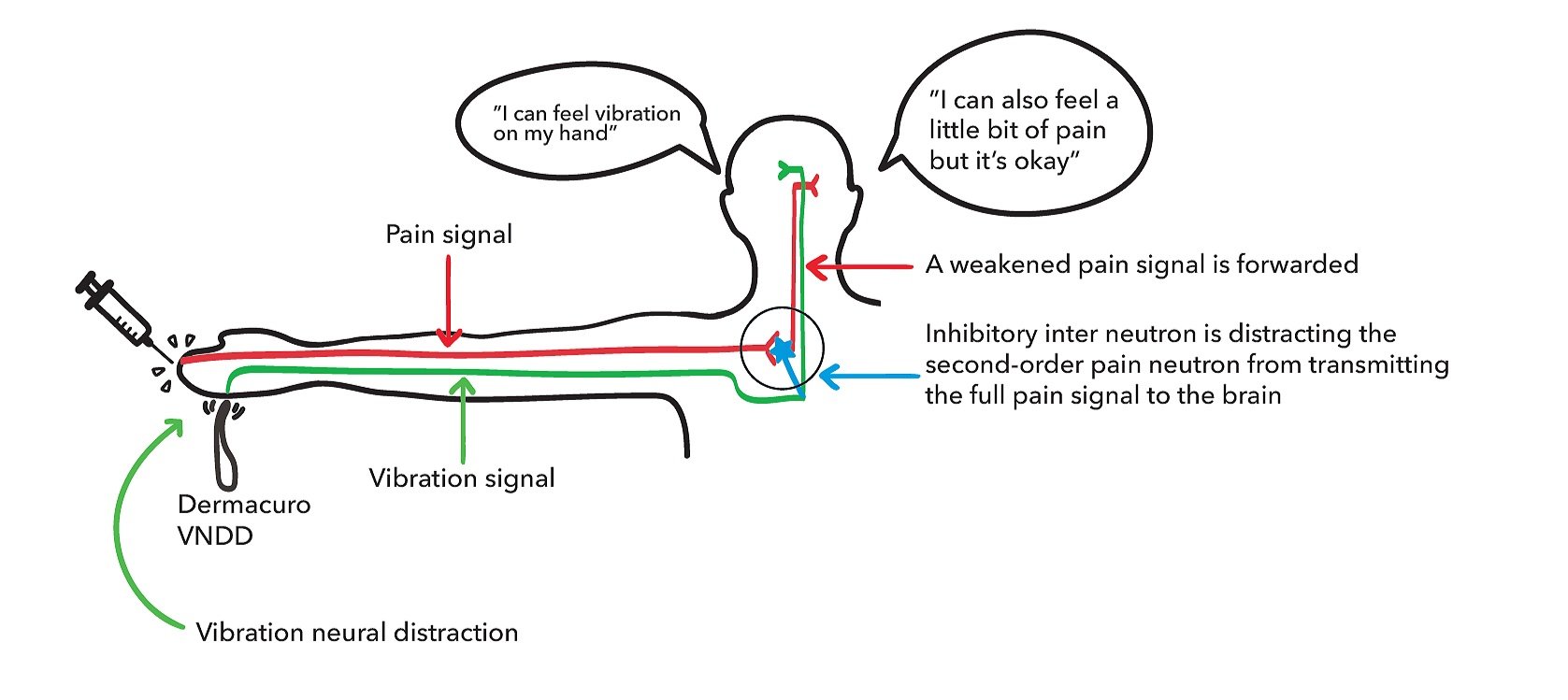
The Vibration Neural Distraction Device is used to minimise patient's sensitivity to pain. The flat-shaped vibrating head rests gently on the skin near the needle entry point and provides mild vibration in the surrounding tissue resulting in neural distraction to minimise pain sensation from the superficial (usually painful) procedure.
The AA battery-powered device delivers vibration to the skin which is effective for neural distraction based on a concept known as 'stimulation-induced pain modulation'. The concept of stimulation-induced analgesia was proposed many years ago and originates from the Gate Control Theory of Pain that was first reported in 1965 by Melzack and Wall.
The device is intended for use by doctors, dentists, nurses, podiatrists, physiotherapists and medical imaging technicians to provide pain relief from injection for patients who are having injections or skin penetration procedures.
How does the brain sense different stimuli – needle compared to vibration?
There are different nerve types that convey sensations to the brain:
• Painful sensations such as from a needle prick, stepping on a sharp object, or a cut in the skin are carried along small diameter nerves (nociceptors)
• Non-pain type sensory information such as cold, heat, texture, vibration are carried along large diameter nerves (non-nociceptors)
• The different nerves and the forwarded signals have their individual pathways to the brain, so the brain can register if the signal is detecting potential harm or not
How does the brain perceive painful stimuli vs non-painful stimuli (eg. vibration)?
Nociception is term to describe the detection of painful stimuli. Nociceptors are specific receptors within the skin, muscle, skeletal structures, and viscera that detect potentially damaging stimuli. The nociceptive inputs are designed to alert the brain of potential dangers that could cause harm – eg: skin penetration – cutting or pricking, extreme heat, cold, mechanical, or chemical signals.
For non-painful stimuli, the sensory conduction pathway through mechanoreceptors in the skin allows for cognitive recognition of vibration. This occurs through afferent neurons, also known as sensory neurons.
How does the VNDD work to reduce pain?
Perception of pain is not simply due to activation of nociceptors, but is the outcome of modulation of both nociceptive and non-nociceptive inputs. If nociceptive (painful) signals outweigh non-nociceptive (non-painful) signals, a pain signal is propagated to the brain. However if non-nociceptive (non-painful) signals outweigh nociceptive (painful) signals, the pain signal to the brain is reduced.
How does the vibration reduce pain sensation?
Vibration has been considered as a pain reduction method for a variety of uses for over 50 years - in dentistry, superficial surgery; skin and deeper injections and early stages of labour. The vibration neural distraction works by using a concept known as ‘stimulation-induced pain modulation’. The concept of stimulation-induced analgesia was proposed many years ago and originates from the Gate Control Theory of Pain that was first reported in 1965 by Melzack and Wall.
The theory states: when A-β fibres (large fibres) are stimulated by non-noxious stimuli, they prevent pain signals transmitted by A-δ or C fibres (small fibres) from reaching the central nervous system. As a result, the non-noxious stimulus suppresses pain.
Summary – the vibration stimulus (non-nociceptive) may inhibit smaller A-δ and C fibre (nociceptive) inputs from a needle injection.
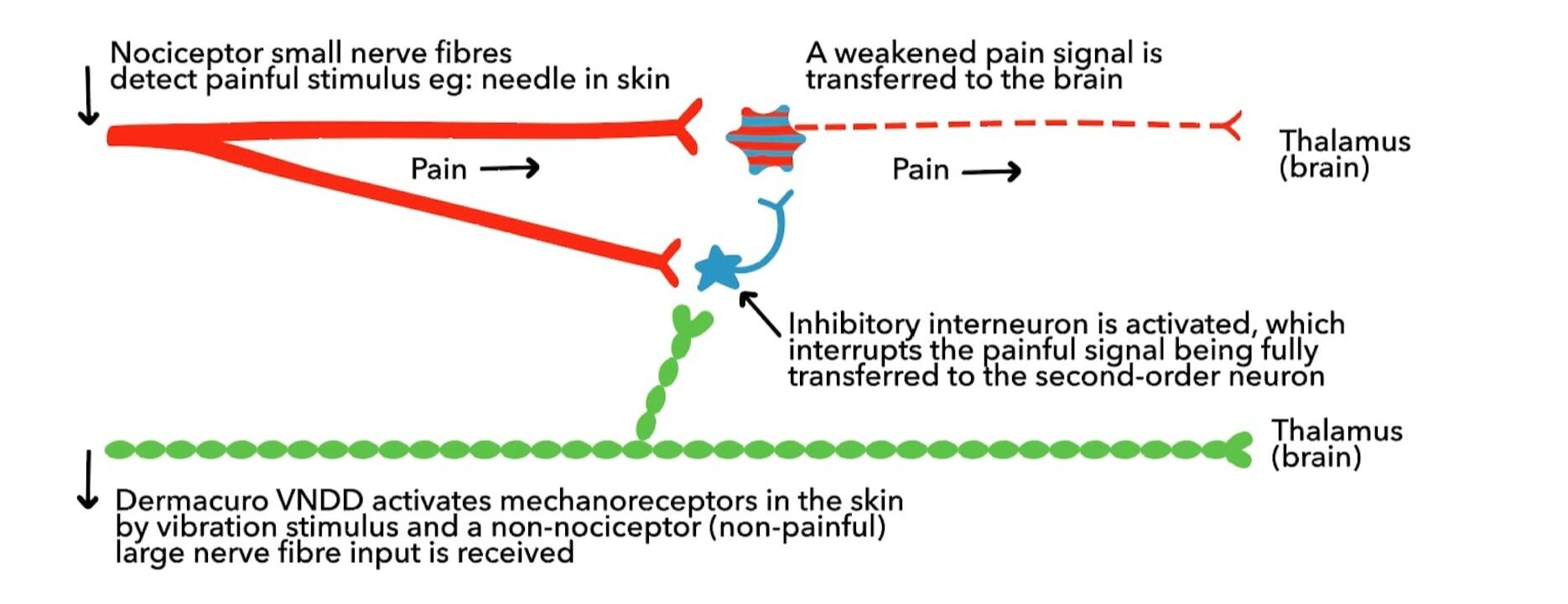
Gate Control Theory of Pain
Even though the different nerves and the forwarded signals have their individual pathways to the brain fortunately the painful sensation nerve pathway can be disrupted by being occupied with receiving signals from the non-pain nerve pathway.
This ‘disruption’ or ‘distraction’ is possible because of the neuron connection between the small (pain) and large(non-pain) neurons within the spine. This connection is known as the ‘inhibitory interneuron’, and it is this neuronal connection that is used to reduce the pain sensation being transmitted to the brain.
According to the Gate Theory of Pain, inhibitory interneurons regulate the transmission of ascending nociceptive (painful) information at the level of the second order neuron, allowing modulation of the pain signal forwarded to the brain.
Is it a TGA approved medical device?
Yes. The Dermacuro Vibration Neural Distraction Device is entered in to the TGA’s ARTG register as a Class I medical device.
What are the typical uses of the VNDD?
Any procedure that induces pain because of skin penetration eg:
Superficial minor surgical procedures
Venepuncture for blood collection
Immunisations
Aesthetic injection procedures eg: Muscle relaxers, Filler; especially in areas where the skin can’t be easily numbed with topical local anaesthetic.
Intra-oral for dental injections (with suitable infection control protocols)
Joint or tendon injections eg: in radiology, sports medicine or orthopaedics
Microneedling or dry-needling procedures
Podiatry procedures
Suture removal, drain removal
IV cannula insertion
What does the research show?
According to a study by Dr Sharma and colleagues published in Aesthetic Surgery Journal, patients experienced both a clinically and statistically significant pain reduction when a vibration stimulus was co-administered with dermal injections. The majority of the clients (86%) reported a preference for vibration distraction for subsequent injections.
How do patients feel about using the VNDD for pain relief?
85% of patients will find the vibration device can reduce the pain sensation by up to 50%, 10% will find it does not change the pain sensation and 5% of patients do not like the vibration sensation. The device may have a particularly beneficial effect in patients who are anxious about the injection procedure or have a low pain tolerance.
What Patients are Saying:
“Made me focus on something other than the needles so I felt less anxious.”
“I had something to do during the procedure which helped to occupy my thoughts on something other than the needles.”
“Significantly reduced the pain from the injections.”
“Loved it - I’m using it for every aesthetic procedure that involves a needle.”
“I’m allergic to some local anaesthetics so this device makes my procedures far less uncomfortable.”
Advantages of using vibration neural distraction during injections
Safe and effective to achieve local pain relief
Maximise patient comfort and reduce anxiety related to injections
Easy application, rapid onset, and good patient acceptance
Provides a highly statistically and clinically significant beneficial effect in terms of patients’ assessment of pain.
Non-pharmacology pain relief option
Nil clearance time – unlike inhalation, oral and injection type pain relief
Affordable – low cost equipment purchase and reusable
Instructions for use
Please be aware that this device will be used as shared clinical equipment and appropriate precautions should be followed to minimise contamination between patients
Use one AA battery
Place vibrating device within a finger of a single use glove (check for latex allergy first). Suggest taping extra glove fingers with micropore so the glove covering remains tight on the device.
Discuss use with patient and trial on a section of their inner forearm so that they know what it will feel like. Power button is located to the side of the device
Then place tip of device close to the area (ideally within 3-5cm distance from skin entry position) before injection.
The neural distraction works best if the device is placed proximal to the injection site (between the injection site and the spine). Need to consider the nerve pathway back to the spine from the injection site.
Turn on and use for a few seconds before injecting or skin penetration commences.
When injection ceases and pain from injection subsides, remove from skin and turn off.
For aesthetic injections, the device can be held by the patient and moved as required with instructions from the injector. Some injectors like to use it in one hand to help stretch or tension the skin near to their injection site.
Disinfect as per shared clinical equipment cleaning protocol between uses
For further information, practitioners are encouraged to Contact Us
References
Fayers, T., Morris, D. S., & Dolman, P. J. (2010). Vibration-assisted anesthesia in eyelid surgery. Ophthalmology, 117(7),
Govas, P., Kazi, R., Slaugenhaupt, R. M., & Carroll, B. T. (2019). Effect of a Vibratory Anesthetic Device on Pain Anticipation and Subsequent Pain Perception Among Patients Undergoing Cutaneous Cancer Removal Surgery: A Randomized Clinical Trial. JAMA Facial Plastic Surgery, 21(6),
Guney, K., Sezgin, B., & Yavuzer, R. (2017). The efficacy of vibration anesthesia on reducing pain levels during lip augmentation: worth the buzz?. Aesthetic Surgery Journal, 37(9)
Li, Y., Dong, W., Wang, M., & Xu, N. (2017). Investigation of the Efficacy and Safety of Topical Vibration Anesthesia to Reduce Pain From Cosmetic Botulinum Toxin A Injections in Chinese Patients: A Multicenter, Randomized, Self-Controlled Study. Dermatologic Surgery, 43
Kuwahara, H., & Ogawa, R. (2016). Using a Vibration Device to Ease Pain During Facial Needling and Injection. Eplasty,
Mally, P., Czyz, C. N., Chan, N. J., & Wulc, A. E. (2014). Vibration anesthesia for the reduction of pain with facial dermal filler injections. Aesthetic Plastic Surgery, 38(2),
Nanitsos, E., Vartuli, R., Forte, A., Dennison, P. J., & Peck, C. C. (2009). The effect of vibration on pain during local anaesthesia injections. Australian Dental Journal.
Özucer, B., & Çam, O. H. (2020, June). A clinical comparison of Emla cream and vibratory anesthetic device application for alleviation of pain associated with botulinum toxin injection for the masseter muscle hypertrophy. Elektronik Kulak Burun Boğaz ve Baş Boyun Cerrahisi Dergisi (Vol. 19, No. 2).
Park, K. Y., Lee, Y., Hong, J. Y., Chung, W. S., Kim, M. N., & Kim, B. J. (2017). Vibration anesthesia for pain reduction during intralesional steroid injection for keloid treatment. Dermatologic Surgery, 43(5)
Pedersen, C., Miller, M., Xu, K. T., Carrasco, L., Smith, C., & Richman, P. B. (2017). Use of a dental vibration tool to reduce pain from digital blocks: a randomized controlled trial. Regional Anesthesia & Pain Medicine, 42(4)
Ramezani, G. H., Tajjedin, M., Valaee, N., & Ebrahimi, H. (2017). Effect of vibration on pain during Injection of local anesthesia: A split-mouth randomized clinical trial. Bioscience Biotechnology Research Communications, 10(4)
Sharma, P., Czyz, C. N., & Wulc, A. E. (2011). Investigating the efficacy of vibration anaesthesia to reduce pain from cosmetic botulinum toxin injections. Aesthetic surgery journal, 31(8)
Smith, K. C., Comite, S. L., Balasubramanian, S., Carver, A., & Liu, J. F. (2004). Vibration anaesthesia: a noninvasive method of reducing discomfort prior to dermatologic procedures. Dermatology Online Journal
Ueki, S., Yamagami, Y., & Makimoto, K. (2019). Effectiveness of vibratory stimulation on needle-related procedural pain in children: a systematic review. JBI database of systematic reviews and implementation reports, 17(7)
Ungor, C., Tosun, E., Dayisoylu, E. H., Taskesen, F., & Senel, F. C. (2014). The effects of vibration on pain and anxiety during local anesthesia administration. JSM Dent, 2(1), 1022.
Wexler, S. J., & Wulc, A. E. (2015). Pain reduction using vibration in aesthetic injections and in eye and facial plastic surgery. In Pearls and Pitfalls in Cosmetic Oculoplastic Surgery (pp. 43-45). Springer, New York, NY.